Practice Policies & Patient Information
Chaperone Policy
Why do we use chaperones in clinical practice?
Comments, Suggestions & Complaints
We are always looking for ways to improve the care we give our patients and from time to time we will carry out some surveys. We would appreciate your cooperation in helping us with these surveys by completing the forms when they are given to you.
Should you have a complaint about any matter, please ask the Receptionist for our Complaints Pack or you can download our complaints pack by clicking here, which details our complaints procedure. We aim to abide by not only regulations but best practice so that patients feel able to make a complaint, please see this diagram for further information by clicking here. In summary – we try to adopt these 5 principles
I felt confident to speak up
I felt that making my complaint was simple
I felt listened to and understood
I felt that my complaint made a difference
I would feel confident making a complaint in the future
NHS Choices has a very full and informative guide about how to complain about a range of NHS services, follow the link here http://www.nhs.uk/choiceintheNHS/Rightsandpledges/complaints/Pages/AboutNHScomplaints.aspx
NHS England have also produced guidance to help you complain about any NHS service, please follow this link for further information
The Patients Association is a national charity concerned with speaking up for patients rights. They can also offer support and guidance. You can reach their website here
Healthwatch Solihull can also be contacted for support and are interested in feedback on all local health and social services . Commissioned by Solihull Council, Healthwatch is tasked with ensuring that the views and experiences of local people are heard by those who plan, run and regulate health and care services. Their website is here
We would appreciate the opportunity to resolve any complaints directly however the following organisations are also available for support:
NHS England -0300 311 22330121 713 87830345 015 40330300 456 23700121 706 4696Send Us Feedback Online
Solihull Clinical Commissioning Group -0300 311 22330121 713 87830345 015 40330300 456 23700121 706 4696Send Us Feedback Online
Parliamentary & Health Services Ombudsman -0300 311 22330121 713 87830345 015 40330300 456 23700121 706 4696Send Us Feedback Online
PowHer – Patient Advocacy Services -0300 311 22330121 713 87830345 015 40330300 456 23700121 706 4696Send Us Feedback Online
Solihull Action through Advocacy specialise in supporting patients with Learning Difficulties – for more details, please visit their website here or telephone 0300 311 22330121 713 87830345 015 40330300 456 23700121 706 4696Send Us Feedback Online
Please use the form below to send us your feedback online:
CQC
This page gives information about the statutory details we are required to make available to the Care Quality Commission. We were last inspected on 15 January 2019 rated ‘Outstanding’ and reviewed 26 March 2020 and retained the rating of ‘Outstanding’ full details of our rating can be found on our home page.
Registration details
Partners
Dr Stephen Cowles, Dr Brian Crichton, Dr Alison Matthews, Dr Nick Ridge, Dr Amit Banerjee, Dr Struthi Gowda
CQC register Hobs Moat Medical Centre to carry out the following legally regulated activities.
Maternity and midwifery services
Terms of this registration relating to carrying out this regulated activity
The registered provider must ensure that the regulated activity Maternity and midwifery services is managed by an individual who is registered as a manager in respect of that activity at or from all locations.
Registered services
Family planning services
Terms of this registration relating to carrying out this regulated activity
The registered provider must ensure that the regulated activity Family planning is managed by an individual who is registered as a manager in respect of that activity at or from all locations.
Registered services
Treatment of disease, disorder or injury
Terms of this registration relating to carrying out this regulated activity
The registered provider must ensure that the regulated activity Treatment of disease, disorder or injury is managed by an individual who is registered as a manager in respect of that activity at or from all locations.
Registered services
Surgical procedures
Terms of this registration relating to carrying out this regulated activity
The registered provider must ensure that the regulated activity Surgical procedures is managed by an individual who is registered as a manager in respect of that activity at or from all locations.
Registered services
Diagnostic and screening procedures
Terms of this registration relating to carrying out this regulated activity
The registered provider must ensure that the regulated activity Diagnostic and screening procedures is managed by an individual who is registered as a manager in respect of that activity at or from all locations.
Registered services
Details of this locations CQC registration
Here you will find the list of services and areas where we, the Care Quality Commission, authorise and regulate this service to operate
Type of service
- Doctors/GPs
Specialisms/services
- Services for everyone
Local authority
- Solihull
Regulated services/activities
CQC register Hobs Moat Medical Centre to carry out the following legally regulated services here:
Maternity and midwifery services
- Dr Brian Crichton is the registered manager for these services at this location.
Family planning services
- Dr Brian Crichton is the registered manager for these services at this location.
Treatment of disease, disorder or injury
- Dr Brian Crichton is the registered manager for these services at this location.
Surgical procedures
- Dr Brian Crichton is the registered manager for these services at this location.
Diagnostic and screening procedures
- Dr Brian Crichton is the registered manager for these services at this location.
Fees for information outside of NHS clinical work
This includes all information that is required for a doctor to complete for any private purpose outside of NHS Hospitals and other signposted health centres within the NHS family such as private health insurance, solicitors paperwork, schools, holidays, fitness for sport, passports etc.
*BMA – British Medical Association
- Letter – to whom it may concern (signed and stamped) £40
- Claim form (private health – sickness accident) £50-£150
- Holiday cancellation insurance form/letter £60
- Fitness to travel letter £60
- Private sick note (not SSP) £40
- Childminder health form £100
- Report on pro forma £100 (no examination)
- Report on pro forma £150 (with examination)
- DVLA reports £85 – £150
- Fitness to participate e.g. Camp America forms £50
- Power of attorney (with consultation) £180
- Private Medical Examination £175
- Firearms £250
You may ask yourself……Surely the doctor is being paid anyway?
“It is important to understand that many GPs are not employed by the NHS. They are self-employed and they have to cover their costs – staff, buildings, heating, lighting, etc. The NHS covers NHS work only. Time spent completing forms and preparing reports takes the GP away from their patients NHS medical care.
When a doctor signs a certificate or completes a report, it is a condition of the Medical Register that they only sign what they know to be true. In order to complete forms the doctor might have to check the patient’s entire medical record. Carelessness or an inaccurate report can have serious consequences for the doctor with the General Medical Council (the doctors’ regulatory body) or even the Police.”
In accordance with our contractual obligations we are publishing our average GP earnings which are £57,689 for 2014/15. We have nine doctors working in the practice, two full time with seven part time occasionally assisted by locum GPs who cover holiday periods.
For the financial year 2015/16
All GP practices are required to declare the mean earnings (e.g. average pay) for GPs working to deliver NHS services to patients at each practice. The average pay for GPs working in Hobs Moat Medical Centre in the last financial year was £26,420 before tax and NI. This calculation is for 2 full-time GPs and 7 part-time GP .
Our Commitment to Equality
This page will provide you with information regarding our commitment to providing our patients with equal opportunity. There is also a section on costings for work outside of the doctor’s NHS contracted protocol this would include supporting medical reports for work, housing, school, DVLA etc. These are also subject to the doctor’s discretion based on the national BMA (British Medical Association) charges.
- Our commitment to equality framework
- Publication Scheme
- Practice charges for non clinical work
Accessible Information Standard
——————————————–
Our Commitment to Equality and Patient Experience
Equality Objectives 2015 & NHS Patient Experience Framework
The Equality Act 2010 places certain responsibilities on public sector organizations such as hospitals.
These are:
- To eliminate unlawful discrimination, harassment and victimization
- Advance equality of opportunity between people who share a relevant protected characteristic and people who do not
- Foster good relations between people who share a relevant protected characteristic and people who do not
- To publish equality objectives at least every four years
- Provide information to demonstrate their compliance with the equality duty at least annually
Currently the public sector Equality Duty applies to all public authorities, including NHS organizations, so covers acute hospitals, primary care trusts, strategic health authorities, mental health and community trusts, ambulance trusts and all foundation trusts.
So what does this mean for our Practice – well at present, there is no obligation for us to publish Equality Objectives. However we take our responsibilities seriously and share the ethos of this initiative. Therefore we offer this commitment to our staff and patients:
“that we will not discriminate against any person on the grounds of”:
- Age
- Disability
- Gender reassignment
- Pregnancy and maternity
- Race – this includes ethnic or national origins, colour or nationality
- Religion or belief – this includes lack of belief
- Gender
- Sexual orientation
Furthermore the practice, in accordance with the Equality Act, also explicitly recognizes that disabled peoples’ needs may be different from those of non-disabled people.
For example, our practice premises are audited each year to ensure that we comply with the requirements of the Equality Duty Act. So we provide disabled car parking spaces, lowered section of our reception desk, hearing loop and wheelchair accessibility. In addition, the Practice Manager has attended specific training around the needs of patients who are partially sighted or blind, those with learning disabilities patients who are hearing impaired. This training has been cascaded through the staff team. The records of those patients are duly noted in order to prompt the reception team to offer additional help as required.
The practice has a range of policies that apply to all staff and visitors to the building, which cover every aspect of our duties under the Equality Act. These ensure that all our staff are treated fairly and without discrimination in any form.
For our patients, we will not discriminate in the offer of admission to our practice list, treatment or service. The only limitation (not covered by the Equality Duty Act) is that of geographical location. This is to ensure that we are able to offer a full service, so meeting the Health & Social Care Bill requirement to provide local services for local people.
Through Solihull CCG, the local clinical commissioning group, we will try to ensure that any decisions about policies, service improvement or implementation take account of disabled peoples’ needs through appropriate consultation. When Solihull CCG became a legal entity in its own right, it keeps a responsibility under the Act, to publish its own Equality Policy and Objectives.
In order to do this they are basing their objectives on the equality information that they collect. For example, the police authority when reviewing its policy on hate crime finds that 68% of all hate crime reported is described as being homophobic. It would therefore make sense for the police authority to publish an objective on how it is to address hate crime.
For us, we do not have this style of data and therefore, apart from making a general commitment to you, our patients, it is hard for us to be able to set specific objectives. We do take into account all comments, suggestions and complaints when reviewing our service provision. We would encourage any patient who feels that we have not met our commitment, to contact the Practice Manager to discuss their concerns. We are fully committed to improving all aspects of the services we offer, but are unable to do this without your help and feedback. If you would like to take this a step further you are very welcome to join our Patient Participation Group.
We are also committed to supporting the NHS Patient Experience Framework. In October 2011, the NHS Quality team agreed on some measures to help the NHS measure patient experience of services. The framework or objectives gives details on the main areas where patient experience matters most. These are
- Respect for patient values, preference and needs which include dignity, privacy, an awareness of quality of life issues and to ensure the patient shares in the decision process about their treatment – In the Health & Social Care Bill this is called “no decision about me without me”
- That NHS services will coordinate and integrate with each other to provide you with a smooth transfer between services, for example when your GP refers you to a hospital consultant
- Information, communication and education – so to make sure we tell other clinical staff enough about you for them to be able to treat you effectively, tell you your results and treatments and help you to look after yourself
- Physical comfort – this means things like helping patients with pain management and relief to ensuring our practice premises are clean and comfortable
- Emotional support – to help you understand your condition and treatment so that you do not feel as anxious or frightened, and look at the impact of any illness, on you, your family and your finances
- Welcoming the involvement of family and friends on whom you as a patient might rely, for example a carer
- Transition and continuity – this probably applies mainly to hospital but for your GP it would mean supporting you to becoming independent and self caring after either an illness or operation, or perhaps having been diagnosed with a long term condition such as diabetes
- Access to care – how easy it is to contact us by telephone, book appointments and even how long you have to wait to be called by the doctor for your appointment. We already undertake patient surveys every year around this topic and are always striving to improve.——————————————————-
Publication Scheme
Information available from Hobs Moat Medical Centre (providing personal medical services under contract to the NHS) under the Freedom of Information Act model publication scheme
Information covered by this scheme is only about the primary, general or personal medical services we provide under contract to the National Health Service.
Please note that where a fee is chargeable, this is made using the guidance in ‘Fees Regulations’ under the Freedom of Information Act published by the Information Commissioner’s Office (Version 1 October 2008)
| Information to be published | How the information can be obtained(eg hard copy, website) | Cost |
| Class1 – Who we are and what we do
The six partners of this Practice are Dr Stephen Cowles, Dr Brian Crichton, Dr Alison Matthews, Dr Nick Ridge, Dr Amit Banerjee and Dr Struthi Gowda. The partners are independent contractors who have an individual contract with Solihull Care Trust to provide primary care services for registered patients of the Practice. Please note some information will be withheld, including personal, confidential information about individuals, which is protected by the Data Protection Act |
Website at www.hobsmoatmedicalcentre.co.uk
|
Free
|
| Our contact details are:
E mail requests can be made via our Practice Manager, Sandra Reynolds on sandra.reynolds@nhs. |
Hobs Moat Medical Centre Ulleries Road Solihull West Midlands B92 8EDTelephone 0121 742 5211 Fax 0121 722 8000
|
|
| Open Times
Closed during bank holidays |
We open Monday to Friday 8am to 6.30pm | |
| We have 2 assistant doctors working at the Practice, a team of Practice nurses supported by a Health Care Assistant, reception and administration staff and associated clinical staff such as midwives, physiotherapists, Health Visitors and Speech and Language therapists | Details of our staff can be found on our website or in our Practice Leaflet | Free |
| Class 2 – What we spend and how we spend it
(Financial information relating to projected and actual income and expenditure, procurement, contracts and financial audit) Current and previous financial year as a minimum |
We produce annual accounts each year, however, these contain details of income that falls outside of this publication scheme. We will provide details of NHS income and how we spend it on request in writing addressed to Sandra Reynolds, Practice Manager | Free |
| Total cost to the PCT/LHB/HSSB of our contracted services. | As above | |
| Audit of NHS income | As above | |
| Class 3 – What our priorities are and how we are doing
(Strategies and plans, performance indicators, audits, inspections and reviews) Current and previous year as a minimum |
We have a 3 year business plan which can be obtained on request in writing
|
Free
|
| Plans for the development and provision of NHS services | We are part of a local Practice Based Commissioning consortium aiming to improve both the services and access in South Solihull. You may ask to see the business plan by writing to Sandra Reynolds, care of the Practice | Free |
| Class 4 – How we make decisions
(Decision making processes and records of decisions) Current and previous year as a minimum |
We make decisions as a Practice or partnership based on our best judgement of what would bring most benefit to our patients | |
| Records of decisions made in the practice affecting the provision of NHS services | Records of major decisions are kept in the form of Practice meeting minutes – you may ask for a copy of these, but you will only be provided with the sections of the minutes that relate to decisions made about how we spend NHS income or what services we intend to provide under the terms of our contract | Free |
| Class 5 – Our policies and procedures
Current written protocols, policies and procedures for delivering our services and responsibilities |
||
| Policies and procedures about the employment of staff | Held | 10p per sheet copied |
| Internal instructions to staff and policies relating to the delivery of services | Held | As above |
| Equality and diversity policy | Held | As above |
| Health and safety policy | Held | As above |
| Complaints procedures (including those covering requests for information and operating the publication scheme) | Held | As above |
| Records management policies (records retention, destruction and archive) | Held | As above |
| Data protection policies | Held | As above |
| Policies and procedures for handling requests for information | Held | As above |
| Patients’ charter | Held | As above |
| Class 6 – Lists and Registers
Currently maintained lists and registers only |
Not applicable | |
| Any publicly available register or list (if any are held this should be publicised; in most circumstances existing access provisions will suffice) | ||
| Class 7 – The services we offer(Information about the services we offer, including leaflets, guidance and newsletters produced for the public)
Current information only |
Our website provides the majority of information about our Practice. However, you can also obtain a practice leaflet from reception along with copies of our most recent newsletters. | Free |
| The services provided under contract to the NHS | ||
| Charges for any of these services | No charges are made for services falling within the scope of the NHS. However, certain vaccinations are not covered by the NHS. Where charges apply, you will be advised of this in advance of treatment | |
| Information leaflets | Freely available in our waiting room | |
| Out of hours arrangements | Solihull Care Trust are responsible for the Out of Hours Services in this area |
We welcome suggestions about how the publications themselves might be improved.
Any questions, comments or complaints about this Scheme should be sent in writing to the Practice Manager at Hobs Moat Medical Centre.
If you have a complaint about the operation of the combined Publication Scheme, or how we have dealt with your request for information from the Scheme, please write to the Practice Manager at Hobs Moat Medical Centre. If you feel that we have not dealt with your complaint adequately, you may take the complaint further to the Information Commissioner. Details of how to do this are available from the Practice Manager at Hobs Moat Medical Centre, Ulleries Road, Solihull West Midlands, B90 8ED.
Fees for information outside of NHS clinical work
Fees for information outside of NHS clinical work
This includes all information that is required for a doctor to complete for any private purpose outside of NHS Hospitals and other signposted health centres within the NHS family such as private health insurance, solicitors paperwork, schools, holidays, fitness for sport, passports etc.
*BMA – British Medical Association
INSURANCE BMA Prices OUR PRICES
Private Medical Claim Forms for completion £60.50 £35.00
Accident/Benefit Claim Form £60.50 £35.00
Holiday Cancellation or Insurance Forms £60.50 £35.00
TRAVEL
Fitness to Travel even with a medical condition £60.50 £40.00
Hepatitis B injections £35 each or £105 course
Certificate for MenACWy £35 certificate and injection
Private Prescriptions £10 charge for prescription and additional charge for drug at pharmacy
MISCELLANEOUS
Private Sick Note £60.50 £30.00
(incapacity certificate, required by a patient for employer)
Fitness for sport £60.50 £30.00
(a patient wishes to exercise with a known medical condition)
Unfit for sport £60.50 £40.00
(a patient wishes to be exempt from private contracts due to sickness, i.e gym membership, booked events etc..)
HGV examination and report £136.00 £85.00
Health reports (on a questionnaire no examination) £86.00 £70.00
Health report (detailed written opinion on patient, no examination) £128.00 £95.00
Straightforward certificate of fact £17.00 £17.00
Extract of medical report £50.00 £10.00
You may ask yourself……Surely the doctor is being paid anyway?
“It is important to understand that many GPs are not employed by the NHS. They are self-employed and they have to cover their costs – staff, buildings, heating, lighting, etc. The NHS covers NHS work only. Time spent completing forms and preparing reports takes the GP away from their patients NHS medical care.
When a doctor signs a certificate or completes a report, it is a condition of the Medical Register that they only sign what they know to be true. In order to complete forms the doctor might have to check the patient’s entire medical record. Carelessness or an inaccurate report can have serious consequences for the doctor with the General Medical Council (the doctors’ regulatory body) or even the Police.”
Patients’ Charter
We aim to give our patients a high quality service and support the NHS Constitution.
Your health is our concern, but your responsibility.
ALL MEMBERS OF THE SURGERY PRIMARY CARE TEAM ARE DEDICATED TO A QUALITY POLICY TO ACHIEVE HEALTH SERVICES WHICH MEET THE PATIENT’S REQUIREMENTS. We are regulated by the Care Quality Commission and provide care and treatment in accordance with national, local and NICE guidance
We are trying to improve how we communicate with patients. Please let us know if you need information in a different format, or you need communication support. This is in accordance with the NHS Accessible Information Specification.
Practice Leaflet:
All new patients will receive a copy of our practice leaflet and copies will be displayed at the reception desk.
Surgery Premises:
Our surgery building will be welcoming, easy for patients to find their way around and appropriate to the needs of users, including the disabled. They will meet all necessary infection control and prevention standards.
Patients’ rights to General Medical Services:
Patients have the rights to:
- be registered with a General Practitioner
- to consult with a GP of their choice
- be offered a health check on joining the practice
- receive urgent care at any time from the practice
- receive appropriate drugs and medicines
- be referred to a specialist if they and the GP agree
- have the right to view their medical records, subject to the Acts and associated procedure, and to know that those working for the NHS are under legal obligation to keep the contents confidential.
|
This Surgery believes in Fairness and Equality and above all, values diversity in all our work as a provider of health services. We will not discriminate against any person on the grounds of race, gender, sexual orientation, age, disability, religion, pregnancy or gender reassignment
|
Changes to Procedures:
When changes are introduced to practice procedures that affect patients, we will ensure that these are clearly explained, by means of a brochure; waiting room noticeboard or individual leaflets, giving as much notice as practicable.
Repeat Prescriptions:
Please allow 48 working hours for repeat prescriptions.
Referrals:
- Urgent referrals to other health and social care agencies will be made within one working day of the patient consultation. Where requested, our GPs will refer you to a private health provider.
- We will normally process non-urgent referrals within five working days of the patient consultation or the doctor’s decision to refer.
Test Results & Diagnostic Assessments
When a doctor or nurse arranges for a test to be taken the patient will be informed how to obtain the result.
Transfer of Medical Records:
The Practice will endeavour to dispatch any medical record required by the Health Authority within seven working days and same day if the request is urgent.
Privacy and Confidentiality:
We will respect our patients’ privacy, dignity and confidentiality at all times.
We provide a confidential service to everyone, including under 16s. This means that you can tell others about your visit, but we won’t. The only reason why we might have to consider passing on your confidential information, would be
to protect you or someone else from serious harm. We would always try to discuss this with you first.
Appointments:
With a Doctor: For routine consultations we will endeavour to offer patients an appointment within two working days of the request. For medically urgent requests, we will offer an appointment on the same day.
With a Practice Nurse: For routine appointments we will offer an appointment within five working days.
When you check in for your appointment using our self check in screen, you will be informed of any anticipated delay to being seen at your appointment time.
Home Visits:
We are unable to guarantee a specific doctor will visit you as this depends on availability and other factors. The decision to home visit will be at the doctors’ discretion.
Our Dignity Challenge
We support the national campaign to promote best standards of care relating to adults and children who may be at risk. This includes having a zero tolerance to all forms of abuse, listening to people to allow them to express their needs and wants, respecting right to privacy and trying to assist people to maintain self esteem while treating each person as an individual.
Out of Hours Emergencies:
We will do everything possible to ensure that our system for contacting the duty doctor is easy to follow, reliable and effective. Please contact 111 when we are closed. Alternatively, these details can be obtained by telephoning our usual number – 0121 742 5211
Waiting Times:
- Surgeries will normally start on time.
- We expect patients to be seen within twenty minutes of their appointment time.
- When a doctor is called away on an emergency we will inform the patients and give them an opportunity to book an alternative appointment, or if preferred, to be seen by another doctor (subject to appointment availability).
With these rights come responsibilities and for the patients this means:
- Courtesy to the staff at all times – remember they are working under doctors’ orders.
- Responding in a positive way to questions asked by the reception staff.
- To attend appointments on time (if you are more than 5 minutes late, you may not be seen – this will be at the discretion of the doctor) or give the practice adequate notice that they wish to cancel. Someone else could use your appointment! For patients who persistently fail to arrive for their appointments, we reserve the right to remove these patients from our list
- An appointment is for one person/one problem only – where another member of the family needs to be seen or discussed, another appointment should be made or a double appointment should be booked if there is more than one concern to be discussed.
- Patients should make every effort when consulting the surgery to make best use of nursing and medical time – home visits should be medically justifiable and not requested for social convenience.
- When patients are asked to give 48 hours notice for repeat prescriptions, please give us this time as it is to allow for accurate prescribing.
- To use emergency out of hours services including 999 and A&E appropriately and not for minor illness or injury
Our Statement of Purpose
The surgery is a GP Partnership, open to all patients living within our practice boundary in Solihull. Please see our location page on our website at www.hobmoatmedicalcentre.co.uk.
From 1st April 2015, we are a General Medical Services (GMS) Practice offering Primary Care services for the diagnosis and prevention of disease. We help patients to manage their health and prevent illness. Our GPs assess, diagnose, treat and manage illness. They carry out screening for some diseases and promote general health and wellbeing. Our GPs act as a patient’s advocate, supporting and representing a patient’s best interests to ensure they receive the best and most appropriate health and/or social care. Our GPs also provide the link to further health services and work closely with other healthcare colleagues. They may also arrange hospital admissions and referrals to other services and specialists and they link with secondary and community services about patient care, taking advice and sharing information where needed.
We are also a training practice involved in the education and training of doctors and have two GP trainers
Locations:
The Practice address is
Hobs Moat Medical Centre
Ulleries Road
Solihull
West Midlands
B92 8ED
Please see our separate document relating to our Mission and Operating statements along with our Improvement priorites
Patient Consent and Confidentiality
The Practice Manager (who is our Caldicott Guardian) is responsible for ensuring your medical records are kept securely and only those staff who need to access your records do so. There are many requests to share patient information that are received every day. So for example, if we refer you to see a specialist at the hospital, we need to send a referral letter to them with detailed information about you and your medical history. We are currently working on an update fair processing notice which is the document that will tell you what we share with whom, and your rights to opt out. The document will be linked to this page in the next few weeks.
If you would like to find out more information or have a specific question, then we have a dedicated email address you can use to contact the practice – solccg.hobsmoatcaldicottguardian.nhs.net
Our Services
The GMS services provided by our GPs are defined under the Standard General Medical Services Contract. These services are mainly split into three groups:
Essential services
We provide essential services for people who have health conditions from which they are expected to recover, chronic disease management and general management of terminally ill patients. Our core services include:
Ø GP consultations
Ø Asthma clinics
Ø Chronic obstructive airways disease clinics
Ø Coronary heart disease clinics
Ø Diabetes clinics
Additional services
Our additional services include:
Ø Cervical cytology screening
Ø Contraceptive services
Ø Child health surveillance
Ø Maternity services
Ø Vaccinations and immunisations
Enhanced services
Our enhanced services include:
Ø Childhood vaccinations and immunisations
Ø Diabetes Management
Ø Minor surgery
Ø Flu immunisation
Ø Minor injury service
Other services
Our Practice also offers services including:
Ø Child health and development
Ø Dressings
Ø Ear wax and syringing
Ø ECGs
Ø End of life care
Ø Epilepsy
Ø Spirometry (Lung tests)
Ø Medication review
Ø Men’s health
Ø Mental health
Ø Pregnancy testing and contraceptive advice
Ø Travel advice
Ø Women’s health
Non-NHS Services
Our Practice also provides services which are non NHS and are paid for by the patient. These services include:
Ø Insurance claims forms
Ø Non NHS vaccinations
Ø Prescription for taking medication abroad
Ø Private sick notes
Ø Pre-employment and HGV medicals
Ø Vaccination certificates
Privacy Notice
Hobs Moat Medical Centre
Data Protection Privacy Notice for Patients
Introduction:
This privacy notice lets you know what happens to any personal data that you give to us, or any information that we may collect from you or about you from other organisations.
This privacy notice applies to personal information processed by or on behalf of the practice.
This Notice explains
- Who we are and how we use your information
- Information about our Data Protection Officer
- What kinds of personal information about you we hold and use (process)
- The legal grounds for our processing of your personal information (including when we share it with others)
- What should you do if your personal information changes?
- For how long your personal information is retained / stored by us?
- What are your rights under Data Protection laws
The UK General Data Protection Regulation (UKGDPR) and the Data Protection Act 2018 (DPA 2018) became law on 25th May 2018, and 1st January 2021 when the UK exited the EU.
For the purpose of applicable data protection legislation (including but not limited to the General Data Protection Regulation (Regulation (UK) 2016/679) (the “UKGDPR”), and the Data Protection Act 2018 the practice responsible for your personal data is Hobs Moat Medical Centre.
This Notice describes how we collect, use and process your personal data, and how in doing so, we comply with our legal obligations to you. Your privacy is important to us, and we are committed to protecting and safeguarding your data privacy rights.
How we use your information and the law.
Hobs Moat Medical Centre will be what’s known as the ‘Controller’ of your personal data.
We collect basic personal data about you and location-based information. This does include name, address and contact details such as email and mobile number etc.
We will also collect sensitive confidential data known as “special category personal data”, in the form of health information, religious belief (if required in a healthcare setting) ethnicity and sex life information that are linked to your healthcare, we may also receive this information about you from other health providers or third parties.
Why do we need your information?
The health care professionals who provide you with care maintain records about your health and any treatment or care you have received previously. These records help to provide you with the best possible healthcare and treatment.
NHS health records may be electronic, paper-based or a mixture of both. We use a combination of working practices and technology to ensure that your information is kept confidential and secure.
Records about you may include the following information;
- Details about you, such as your address, your carer or legal representative and emergency contact details.
- Any contact the surgery has had with you, such as appointments, clinic visits, emergency appointments.
- Notes and reports about your health.
- Details about your treatment and care.
- Results of investigations such as laboratory tests, x-rays etc.
- Relevant information from other health professionals, relatives or those who care for you.
- Contact details (including email address, mobile telephone number and home telephone number)
To ensure you receive the best possible care, your records are used to facilitate the care you receive, including contacting you. Information held about you may be used to help protect the health of the public and to help us manage the NHS and the services we provide. Limited information may be used within the GP practice for clinical audit to monitor the quality of the service we provided.
How do we lawfully use your data?
We need your personal, sensitive and confidential data in order to provide you with healthcare services as a General Practice, under the General Data Protection Regulation we will be lawfully using your information in accordance with: –
Article 6, e) processing is necessary for the performance of a task carried out in the public interest or in the exercise of official authority vested in the controller;”
Article 9, (h) processing is necessary for the purposes of preventive or occupational medicine, for the assessment of the working capacity of the employee, medical diagnosis, the provision of health or social care or treatment or the management of health or social care systems
This Privacy Notice applies to the personal data of our patients and the data you have given us about your carers/family members.
We use your personal and healthcare information in the following ways:
- when we need to speak to, or contact other doctors, consultants, nurses or any other medical/healthcare professional or organisation during the course of your diagnosis or treatment or on going healthcare;
- when we are required by law to hand over your information to any other organisation, such as the police, by court order, solicitors, or immigration enforcement.
- In a de-identified form to support planning of health services and to improve health outcomes for our population
We will never pass on your personal information to anyone else who does not need it, or has no right to it, unless you give us consent to do so.
Legal justification for collecting and using your information
The law says we need a legal basis to handle your personal and healthcare information.
Contract: We have a contract with NHS England to deliver healthcare services to you. This contract provides that we are under a legal obligation to ensure that we deliver medical and healthcare services to the public.
Consent: Sometimes we also rely on the fact that you give us consent to use your personal and healthcare information so that we can take care of your healthcare needs.
Please note that you have the right to withdraw consent at any time if you no longer wish to receive services from us.
Necessary care: Providing you with the appropriate healthcare, where necessary. The Law refers to this as ‘protecting your vital interests’ where you may be in a position not to be able to consent.
Law: Sometimes the law obliges us to provide your information to an organisation (see above).
The law states that personal information about your health falls into a special category of information because it is very sensitive. Reasons that may entitle us to use and process your information may be as follows:
Public Interest: Where we may need to handle your personal information when it is considered to be in the public interest. For example, when there is an outbreak of a specific disease and we need to contact you for treatment, or we need to pass your information to relevant organisations to ensure you receive advice and/or treatment
Consent: When you have given us consent
Vital Interest: If you are incapable of giving consent, and we have to use your information to protect your vital interests (e.g. if you have had an accident and you need emergency treatment)
Defending a claim: If we need your information to defend a legal claim against us by you, or by another party
Providing you with medical care: Where we need your information to provide you with medical and healthcare services
Risk Stratification
Risk stratification data tools are increasingly being used in the NHS to help determine a person’s risk of suffering a condition, preventing an unplanned or (re)admission and identifying a need for preventive intervention. Information about you is collected from several sources including NHS Trusts and from this GP Practice. The identifying parts of your data are removed, analysis of your data is undertaken, and a risk score is then determined. This is then provided back to your GP as data controller in an identifiable form. Risk stratification enables your GP to focus on preventing ill health and not just the treatment of sickness. If necessary, your GP may be able to offer you additional services. Please note that you have the right to opt out of your data being used in this way in most circumstances, please contact the practice for further information about opt out.
Individual Risk Management at a GP practice level however is deemed to be part of your individual healthcare and is covered by our legal powers above.
Sometimes we may provide information about you in an anonymised form. Such information is used analyse population- level heath issues, and helps the NHS to plan better services. If we share information for these purposes, then none of the information will identify you as an individual and cannot be traced back to you.
Medicines Management
The Practice may conduct Medicines Management Reviews of medications prescribed to its patients. This service performs a review of prescribed medications to ensure patients receive the most appropriate, up to date and cost-effective treatments. The reviews are carried out by the CCGs Medicines Management Team under a Data Processing contract with the Practice.
GP Connect Service
The GP Connect service allows authorised clinical staff at NHS 111 to seamlessly access our practice’s clinical system and book directly on behalf of a patient. This means that should you call NHS 111 and the clinician believes you need an appointment with your GP Practice, the clinician will access available appointment slots only (through GP Connect) and book you in. This will save you time as you will not need to contact the practice direct for an appointment.
The practice will not be sharing any of your data and the practice will only allow NHS 111 to see available appointment slots. They will not even have access to your record. However, NHS 111 will share any relevant data with us, but you will be made aware of this. This will help your GP in knowing what treatment / service / help you may require.
Please note if you no longer require the appointment or need to change the date and time for any reason you will need to speak to one of our reception staff and not NHS 111.
Patient Communication
Because we are obliged to protect any confidential information we hold about you and we take this very seriously, it is imperative that you let us know immediately if you change any of your contact details.
We may contact you using SMS texting to your mobile phone in the event that we need to notify you about appointments and other services that we provide to you involving your direct care, therefore you must ensure that we have your up to date details. This is to ensure we are sure we are actually contacting you and not another person. As this is operated on an ‘opt out’ basis we will assume that you give us permission to contact you via SMS if you have provided us with your mobile telephone number. Please let us know if you wish to opt out of this SMS service. We may also contact you using the email address you have provided to us. Please ensure that we have your up to date details.
There may be occasions where authorised research facilities would like you to take part in research. Your contact details may be used to invite you to receive further information about such research opportunities.
Safeguarding
The Practice is dedicated to ensuring that the principles and duties of safeguarding adults and children are holistically, consistently and conscientiously applied with the wellbeing of all, at the heart of what we do.
Our legal basis for processing For the General Data Protection Regulation (GDPR) purposes is: –
Article 6(1)(e) ‘…exercise of official authority…’.
For the processing of special categories data, the basis is: –
Article 9(2)(b) – ‘processing is necessary for the purposes of carrying out the obligations and exercising specific rights of the controller or of the data subject in the field of employment and social security and social protection law…’
Research
Clinical Practice Research Datalink (CPRD) collects de-identified patient data from a network of GP practices across the UK. Primary care data are linked to a range of other health related data to provide a longitudinal, representative UK population health dataset. You can opt out of your information being used for research purposes at any time (see below), full details can be found here: –
https://cprd.com/transparency-information
The legal bases for processing this information
CPRD do not hold or process personal data on patients; however, NHS Digital (formally the Health and Social Care Centre) may process ‘personal data’ for us as an accredited ‘safe haven’ or ‘trusted third-party’ within the NHS when linking GP data with data from other sources. The legal bases for processing this data are:
- Medicines and medical device monitoring: Article 6(e) and Article 9(2)(i) – public interest in the area of public health
- Medical research and statistics: Article 6(e) and Article 9(2)(j) – public interest and scientific research purposes
Any data CPRD hold or pass on to bona fide researchers, except for clinical research studies, will have been anonymised in accordance with the Information Commissioner’s Office Anonymisation Code of Practice. We will hold data indefinitely for the benefit of future research, but studies will normally only hold the data we release to them for twelve months.
Categories of personal data
The data collected by Practice staff in the event of a safeguarding situation will be as much personal information as is possible that is necessary to obtain in order to handle the situation. In addition to some basic demographic and contact details, we will also process details of what the safeguarding concern is. This is likely to be special category information (such as health information).
Sources of the data
The Practice will either receive or collect information when someone contacts the organisation with safeguarding concerns, or we believe there may be safeguarding concerns and make enquiries to relevant providers.
Recipients of personal data
The information is used by the Practice when handling a safeguarding incident or concern. We may share information accordingly to ensure duty of care and investigation as required with other partners such as local authorities, the police or healthcare professionals (i.e. their GP or mental health team).
Third party processors
In order to deliver the best possible service, the practice will share data (where required) with other NHS bodies such as other GP practices and hospitals. In addition, the practice will use carefully selected third party service providers. When we use a third party service provider to process data on our behalf then we will always have an appropriate agreement in place to ensure that they keep the data secure, that they do not use or share information other than in accordance with our instructions and that they are operating appropriately. Examples of functions that may be carried out by third parties include:
- Companies that provide IT services & support, including our core clinical systems; systems which manage patient facing services (such as our website and service accessible through the same); data hosting service providers; systems which facilitate appointment bookings or electronic prescription services; document management services etc.
- Delivery services (for example if we were to arrange for delivery of any medicines to you).
- Payment providers (if for example you were paying for a prescription or a service such as travel vaccinations).
Further details regarding specific third-party processors can be supplied on request to the Data Protection Officer as below.
How do we maintain the confidentiality of your records?
We are committed to protecting your privacy and will only use information collected lawfully in accordance with:
- Data Protection Act 2018
- The General Data Protection Regulations 2016
- Human Rights Act 1998
- Common Law Duty of Confidentiality
- Health and Social Care Act 2012
- NHS Codes of Confidentiality, Information Security and Records Management
- Information: To Share or Not to Share Review
Every member of staff who works for an NHS organisation has a legal obligation to keep information about you confidential.
We will only ever use or pass on information about you if others involved in your care have a genuine need for it. We will not disclose your information to any third party without your permission unless there are exceptional circumstances (i.e. life or death situations), where the law requires information to be passed on and / or in accordance with the information sharing principle following Dame Fiona Caldicott’s information sharing review (Information to share or not to share) where “The duty to share information can be as important as the duty to protect patient confidentiality.” This means that health and social care professionals should have the confidence to share information in the best interests of their patients within the framework set out by the Caldicott principles.
Our practice policy is to respect the privacy of our patients, their families and our staff and to maintain compliance with the General Data Protection Regulation (GDPR) and all UK specific Data Protection Requirements. Our policy is to ensure all personal data related to our patients will be protected.
All employees and sub-contractors engaged by our practice are asked to sign a confidentiality agreement. The practice will, if required, sign a separate confidentiality agreement if the client deems it necessary. If a sub-contractor acts as a data processor for Hobs Moat Medical Centre an appropriate contract (art 24-28) will be established for the processing of your information.
In certain circumstances you may have the right to withdraw your consent to the processing of data. Please contact the Data Protection Officer in writing if you wish to withdraw your consent. If some circumstances we may need to store your data after your consent has been withdrawn to comply with a legislative requirement.
Some of this information will be held centrally and used for statistical purposes. Where we do this, we take strict measures to ensure that individual patients cannot be identified. Sometimes your information may be requested to be used for research purposes – the surgery will always gain your consent before releasing the information for this purpose in an identifiable format. In some circumstances you can Opt-out of the surgery sharing any of your information for research purposes.
With your consent we would also like to use your information
There are times that we may want to use your information to contact you or offer you services, not directly about your healthcare, in these instances we will always gain your consent to contact you. We would however like to use your name, contact details and email address to inform you of other services that may benefit you. We will only do this with your consent. There may be occasions where authorised research facilities would like you to take part on innovations, research, improving services or identifying trends, you will be asked to opt into such programmes if you are happy to do so.
At any stage where we would like to use your data for anything other than the specified purposes and where there is no lawful requirement for us to share or process your data, we will ensure that you have the ability to consent and opt out prior to any data processing taking place.
This information is not shared with third parties or used for any marketing and you can unsubscribe at any time via phone, email or by informing the practice DPO as below.
National Opt-Out Facility
You can choose whether your confidential patient information is used for research and planning.
Who can use your confidential patient information for research and planning?
It is used by the NHS, local authorities, university and hospital researchers, medical colleges and pharmaceutical companies researching new treatments.
Making your data opt-out choice
You can choose to opt out of sharing your confidential patient information for research and planning. There may still be times when your confidential patient information is used: for example, during an epidemic where there might be a risk to you or to other people’s health. You can also still consent to take part in a specific research project.
Will choosing this opt-out affect your care and treatment?
No, your confidential patient information will still be used for your individual care. Choosing to opt out will not affect your care and treatment. You will still be invited for screening services, such as screenings for bowel cancer.
What should you do next?
You do not need to do anything if you are happy about how your confidential patient information is used.
If you do not want your confidential patient information to be used for research and planning, you can choose to opt out securely online or through a telephone service.
You can change your choice at any time. To find out more or to make your choice visit nhs.uk/your-nhs-data-matters or call 0300 303 5678
NHS Digital Data Collection from the Practice
The NHS needs data about the patients it treats to plan and deliver its services and to ensure that care and treatment provided is safe and effective. The General Practice Data for Planning and Research data collection will help the NHS to improve health and care services for everyone by collecting patient data that can be used to do this. For example patient data can help the NHS to:
- monitor the long-term safety and effectiveness of care
- plan how to deliver better health and care services
- prevent the spread of infectious diseases
- identify new treatments and medicines through health research
GP practices already share patient data for these purposes, but this new data collection will be more efficient and effective.
This means that GPs can get on with looking after their patients, and NHS Digital can provide controlled access to patient data to the NHS and other organisations who need to use it, to improve health and care for everyone.
Contributing to research projects will benefit us all as better and safer treatments are introduced more quickly and effectively without compromising your privacy and confidentiality.
NHS Digital has engaged with the British Medical Association (BMA), Royal College of GPs (RCGP) and the National Data Guardian (NDG) to ensure relevant safeguards are in place for patients and GP practices.
NHS Digital purposes for processing patient data
Patient data from GP medical records kept by GP practices in England is used every day to improve health, care and services through planning and research, helping to find better treatments and improve patient care. The NHS is introducing an improved way to share this information – called the General Practice Data for Planning and Research data collection.
NHS Digital will collect, analyse, publish and share this patient data to improve health and care services for everyone. This includes:
- informing and developing health and social care policy
- planning and commissioning health and care services
- taking steps to protect public health (including managing and monitoring the coronavirus pandemic)
- in exceptional circumstances, providing you with individual care
- enabling healthcare and scientific research
Any data that NHS Digital collects will only be used for health and care purposes. It is never shared with marketing or insurance companies.
What patient data NHS Digital collect
Patient data will be collected from GP medical records about:
- any living patient registered at a GP practice in England when the collection started – this includes children and adults
- any patient who died after the data collection started, and was previously registered at a GP practice in England when the data collection started
While 1 September has been seen by some as a cut-off date for opt-out, after which data extraction would begin, Government has stated this will not be the case and data extraction will not commence until NHS Digital have met the tests.
The NHS is introducing three changes to the opt-out system which mean that patients will be able to change their opt-out status at any time:
- Patients do not need to register a Type 1 opt-out by 1 September to ensure their GP data will not be uploaded
- NHS Digital will create the technical means to allow GP data that has previously been uploaded to the system via the GPDPR collection to be deleted when someone registers a Type 1 opt-out
- The plan to retire Type 1 opt-outs will be deferred for at least 12 months while we get the new arrangements up and running, and will not be implemented without consultation with the RCGP, the BMA and the National Data Guardian
We will not collect your name or where you live. Any other data that could directly identify you, for example NHS number, General Practice Local Patient Number, full postcode and date of birth, is replaced with unique codes which are produced by de-identification software before the data is shared with NHS Digital.
This process is called pseudonymisation and means that no one will be able to directly identify you in the data. The diagram below helps to explain what this means. Using the terms in the diagram, the data we collect would be described as de-personalised.
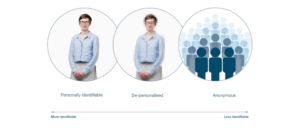
Image provided by Understanding Patient Data under licence.
NHS Digital will be able to use the same software to convert the unique codes back to data that could directly identify you in certain circumstances, and where there is a valid legal reason. Only NHS Digital has the ability to do this. This would mean that the data became personally identifiable data in the diagram above. An example would be where you consent to your identifiable data being shared with a research project or clinical trial in which you are participating, as they need to know the data is about you.
More information about when we may be able to re-identify the data is in the who we share your patient data with section below.
The NHS Digital programme will be providing further information as the programme progresses. In the meantime, if you have any questions, you can contact the programme at enquiries@nhsdigital.nhs.uk.
The NHS Digital web pages also provide further information at https://digital.nhs.uk/data-and-information/data-collections-and-data-sets/data-collections/general-practice-data-for-planning-and-research#additional-information-for-gp-practices.
The Data NHD Digital collect
We will only collect structured and coded data from patient medical records that is needed for specific health and social care purposes explained above.
Data that directly identifies you as an individual patient, including your NHS number, General Practice Local Patient Number, full postcode, date of birth and if relevant date of death, is replaced with unique codes produced by de-identification software before it is sent to NHS Digital. This means that no one will be able to directly identify you in the data.
NHS Digital will be able to use the software to convert the unique codes back to data that could directly identify you in certain circumstances, and where there is a valid legal reason. This would mean that the data became personally identifiable in the diagram above. It will still be held securely and protected, including when it is shared by NHS Digital.
NHS Digital will collect
- data on your sex, ethnicity and sexual orientation
- clinical codes and data about diagnoses, symptoms, observations, test results, medications, allergies, immunisations, referrals and recalls, and appointments, including information about your physical, mental and sexual health
- data about staff who have treated you
More detailed information about the patient data we collect is contained in the Data Provision Notice issued to GP practices.
NHS Digital Does not collect.
- your name and address (except for your postcode in unique coded form)
- written notes (free text), such as the details of conversations with doctors and nurses
- images, letters and documents
- coded data that is not needed due to its age – for example medication, referral and appointment data that is over 10 years old
- coded data that GPs are not permitted to share by law – for example certain codes about IVF treatment, and certain information about gender re-assignment
Opting out of NHS Digital collecting your data (Type 1 Opt-out)
If you do not want your identifiable patient data (personally identifiable data in the diagram above) to be shared outside of your GP practice for purposes except for your own care, you can register an opt-out with your GP practice. This is known as a Type 1 Opt-out.
Type 1 Opt-outs were introduced in 2013 for data sharing from GP practices, but may be discontinued in the future as a new opt-out has since been introduced to cover the broader health and care system, called the National Data Opt-out. If this happens people who have registered a Type 1 Opt-out will be informed. More about National Data Opt-outs is in the section Who we share patient data with.
NHS Digital will not collect any patient data for patients who have already registered a Type 1 Opt-out in line with current policy. If this changes patients who have registered a Type 1 Opt-out will be informed.
If you do not want your patient data shared with NHS Digital, you can register a Type 1 Opt-out with your GP practice. You can register a Type 1 Opt-out at any time. You can also change your mind at any time and withdraw a Type 1 Opt-out.
Data sharing with NHS Digital will start on 1 September 2021.
If you have already registered a Type 1 Opt-out with your GP practice your data will not be shared with NHS Digital.
If you wish to register a Type 1 Opt-out with your GP practice before data sharing starts with NHS Digital, this should be done by returning this form to your GP practice. If you have previously registered a Type 1 Opt-out and you would like to withdraw this, you can also use the form to do this. You can send the form by post or email to your GP practice or call 0300 3035678 for a form to be sent out to you.
If you register a Type 1 Opt-out after your patient data has already been shared with NHS Digital, no more of your data will be shared with NHS Digital. NHS Digital will however still hold the patient data which was shared with us before you registered the Type 1 Opt-out.
If you do not want NHS Digital to share your identifiable patient data (personally identifiable data in the diagram above) with anyone else for purposes beyond your own care, then you can also register a National Data Opt-out. There is more about National Data Opt-outs and when they apply in the National Data Opt-out section below.
NHS Digital legal basis for collecting, analysing and sharing patient data.
When we collect, analyse, publish and share patient data, there are strict laws in place that we must follow. Under the UK General Data Protection Regulation (GDPR), this includes explaining to you what legal provisions apply under GDPR that allows us to process patient data. The GDPR protects everyone’s data.
NHS Digital has been directed by the Secretary of State for Health and Social Care under the General Practice Data for Planning and Research Directions 2021 to collect and analyse data from GP practices for health and social care purposes including policy, planning, commissioning, public health and research purposes.
NHS Digital is the controller of the patient data collected and analysed under the GDPR jointly with the Secretary of State for Health and Social Care.
All GP practices in England are legally required to share data with NHS Digital for this purpose under the Health and Social Care Act 2012 (2012 Act). More information about this requirement is contained in the Data Provision Notice issued by NHS Digital to GP practices.
NHS Digital has various powers to publish anonymous statistical data and to share patient data under sections 260 and 261 of the 2012 Act. It also has powers to share data under other Acts, for example the Statistics and Registration Service Act 2007.
Regulation 3 of the Health Service (Control of Patient Information) Regulations 2002 (COPI) also allow confidential patient information to be used and shared appropriately and lawfully in a public health emergency. The Secretary of State has issued legal notices under COPI (COPI Notices) requiring NHS Digital, NHS England and Improvement, arm’s-length bodies (such as Public Health England), local authorities, NHS trusts, clinical commissioning groups and GP practices to share confidential patient information to respond to the COVID-19 outbreak. Any information used or shared during the COVID-19 outbreak will be limited to the period of the outbreak unless there is another legal basis to use confidential patient information.
The legal basis under UKGDPR for General Practice Data for Planning and Research
How NHS Digital use patient data
NHS Digital will analyse and link the patient data we collect with other patient data we hold to create national data sets and for data quality purposes.
NHS Digital will be able to use the de-identification software to convert the unique codes back to data that could directly identify you in certain circumstances for these purposes, where this is necessary and where there is a valid legal reason. There are strict internal approvals which need to be in place before we can do this and this will be subject to independent scrutiny and oversight by the Independent Group Advising on the Release of Data (IGARD).
These national data sets are analysed and used by NHS Digital to produce national statistics and management information, including public dashboards about health and social care which are published. We never publish any patient data that could identify you. All data we publish is anonymous statistical data.
For more information about data we publish see Data and Information and Data Dashboards.
We may also carry out analysis on national data sets for data quality purposes and to support the work of others for the purposes set out in Our purposes for processing patient data section above.
Who NHS Digital share patient data with
All data which is shared by NHS Digital is subject to robust rules relating to privacy, security and confidentiality and only the minimum amount of data necessary to achieve the relevant health and social care purpose will be shared.
All requests to access patient data from this collection, other than anonymous aggregate statistical data, will be assessed by NHS Digital’s Data Access Request Service, to make sure that organisations have a legal basis to use the data and that it will be used safely, securely and appropriately.
These requests for access to patient data will also be subject to independent scrutiny and oversight by the Independent Group Advising on the Release of Data (IGARD). Organisations approved to use this data will be required to enter into a data sharing agreement with NHS Digital regulating the use of the data.
There are a number of organisations who are likely to need access to different elements of patient data from the General Practice Data for Planning and Research collection. These include but may not be limited to:
- the Department of Health and Social Care and its executive agencies, including Public Health England and other government departments
- NHS England and NHS Improvement
- primary care networks (PCNs), clinical commissioning groups (CCGs) and integrated care organisations (ICOs)
- local authorities
- research organisations, including universities, charities, clinical research organisations that run clinical trials and pharmaceutical companies
If the request is approved, the data will either be made available within a secure data access environment within NHS Digital infrastructure, or where the needs of the recipient cannot be met this way, as a direct dissemination of data. We plan to reduce the amount of data being processed outside central, secure data environments and increase the data we make available to be accessed via our secure data access environment. For more information read about improved data access in improving our data processing services.
Data will always be shared in the uniquely coded form (de-personalised data in the diagram above) unless in the circumstances of any specific request it is necessary for it to be provided in an identifiable form (personally identifiable data in the diagram above). For example, when express patient consent has been given to a researcher to link patient data from the General Practice for Planning and Research collection to data the researcher has already obtained from the patient.
It is therefore possible for NHS Digital to convert the unique codes back to data that could directly identify you in certain circumstances, and where there is a valid legal reason which permits this without breaching the common law duty of confidentiality. This would include:
- where the data was needed by a health professional for your own care and treatment
- where you have expressly consented to this, for example to participate in a clinical trial
- where there is a legal obligation, for example where the COPI Notices apply – see Our legal basis for collecting, analysing and sharing patient data above for more information on this
- where approval has been provided by the Health Research Authority or the Secretary of State with support from the Confidentiality Advisory Group (CAG) under Regulation 5 of the Health Service (Control of Patient Information) Regulations 2002 (COPI) – this is sometimes known as a ‘section 251 approval’
This would mean that the data was personally identifiable in the diagram above. Re-identification of the data would only take place following approval of the specific request through the Data Access Request Service, and subject to independent assurance by IGARD and consultation with the Professional Advisory Group, which is made up of representatives from the BMA and the RCGP. If you have registered a National Data Opt-out, this would be applied in accordance with the National Data Opt-out policy before any identifiable patient data (personally identifiable data in the diagram above) about you was shared. More about the National Data Opt-out is in the section below.
Details of who we have shared data with, in what form and for what purposes are published on our data release register.
Where NHS digital stores patient data
NHS Digital only stores and processes patient data for this data collection within the United Kingdom (UK).
Fully anonymous data (that does not allow you to be directly or indirectly identified), for example statistical data that is published, may be stored and processed outside of the UK. Some of our processors may process patient data outside of the UK. If they do, we will always ensure that the transfer outside of the UK complies with data protection laws.
Where do we store your information electronically?
All the personal data we process is processed by our staff in the UK however for the purposes of IT hosting and maintenance this information may be located on servers within the European Union.
No 3rd parties have access to your personal data unless the law allows them to do so and appropriate safeguards have been put in place such as a Data Processor as above). We have a Data Protection regime in place to oversee the effective and secure processing of your personal and or special category (sensitive, confidential) data.
Who are our partner organisations?
We may also have to share your information, subject to strict agreements on how it will be used, with the following organisations;
- NHS Trusts / Foundation Trusts
- GP’s
- Primary Care Network
- NHS Commissioning Support Units
- Independent Contractors such as dentists, opticians, pharmacists
- Private Sector Providers
- Voluntary Sector Providers
- Ambulance Trusts
- Clinical Commissioning Groups
- Social Care Services
- NHS England (NHSE) and NHS Digital (NHSD)
- Multi Agency Safeguarding Hub (MASH)
- Local Authorities
- Education Services
- Fire and Rescue Services
- Police & Judicial Services
- Voluntary Sector Providers
- Private Sector Providers
- Other ‘data processors’ which you will be informed of
You will be informed who your data will be shared with and in some cases asked for consent for this to happen when this is required.
Computer System
This practice operates a Clinical Computer System on which NHS Staff record information securely. This information can then be shared with other clinicians so that everyone caring for you is fully informed about your medical history, including allergies and medication.
To provide around the clock safe care, unless you have asked us not to, we will make information available to our Partner Organisation (above). Wherever possible, their staff will ask your consent before your information is viewed.
Shared Care Records
To support your care and improve the sharing of relevant information to our partner organisations (as above) when they are involved in looking after you, we will share information to other systems. You can opt out of this sharing of your records with our partners at anytime if this sharing is based on your consent.
We may also use external companies to process personal information, such as for archiving purposes. These companies are bound by contractual agreements to ensure information is kept confidential and secure. All employees and sub-contractors engaged by our practice are asked to sign a confidentiality agreement. If a sub-contractor acts as a data processor for Hobs Moat Medical Centre an appropriate contract (art 24-28) will be established for the processing of your information.
Sharing your information without consent
We will normally ask you for your consent, but there are times when we may be required by law to share your information without your consent, for example:
- where there is a serious risk of harm or abuse to you or other people;
- Safeguarding matters and investigations
- where a serious crime, such as assault, is being investigated or where it could be prevented;
- notification of new births;
- where we encounter infectious diseases that may endanger the safety of others, such as meningitis or measles (but not HIV/AIDS);
- where a formal court order has been issued;
- where there is a legal requirement, for example if you had committed a Road Traffic Offence.
How long will we store your information?
We are required under UK law to keep your information and data for the full retention periods as specified by the NHS Records management code of practice for health and social care and national archives requirements.
More information on records retention can be found online at (https://digital.nhs.uk/article/1202/Records-Management-Code-of-Practice-for-Health-and-Social-Care-2016).
How can you access, amend move the personal data that you have given to us?
Even if we already hold your personal data, you still have various rights in relation to it. To get in touch about these, please contact us. We will seek to deal with your request without undue delay, and in any event in accordance with the requirements of any applicable laws. Please note that we may keep a record of your communications to help us resolve any issues which you raise.
Right to object: If we are using your data and you do not agree, you have the right to object. We will respond to your request within one month (although we may be allowed to extend this period in certain cases). This is NOT an absolute right sometimes we will need to process your data even if you object.
Right to withdraw consent: Where we have obtained your consent to process your personal data for certain activities (for example for a research project, or consent to send you information about us or matters you may be interested in), you may withdraw your consent at any time.
Right to erasure: In certain situations (for example, where we have processed your data unlawfully), you have the right to request us to “erase” your personal data. We will respond to your request within one month (although we may be allowed to extend this period in certain cases) and will only disagree with you if certain limited conditions apply. If we do agree to your request, we will delete your data but will need to keep a note of your name/ other basic details on our register of individuals who would prefer not to be contacted. This enables us to avoid contacting you in the future where your data are collected in unconnected circumstances. If you would prefer us not to do this, you are free to say so.
Right of data portability: If you wish, you have the right to transfer your data from us to another data controller. We will help with this with a GP to GP data transfer and transfer of your hard copy notes.
Primary Care Network
The objective of primary care networks (PCNs) is for group practices together to create more collaborative workforces which ease the pressure of GP’s, leaving them better able to focus on patient care. The aim is that by July 2019, all areas within England will be covered by a PCN.
Primary Care Networks form a key building block of the NHS long-term plan. Bringing general practices together to work at scale has been a policy priority for some years for a range of reasons, including improving the ability of practices to recruit and retain staff; to manage financial and estates pressures; to provide a wider range of services to patients and to more easily integrate with the wider health and care system.
All GP practices are expected to come together in geographical networks covering populations of approximately 30–50,000 patients by June 2019 if they are to take advantage of additional funding attached to the GP contract. This size is consistent with the size of the primary care homes, which exist in many places in the country, but much smaller than most GP Federations.
This means the practice may share your information with other practices within the PCN to provide you with your care and treatment.
Population Health Management
Population Health Management (or PHM for short) is aimed at improving the health of an entire population. It is being implemented across the NHS and this Practice is taking part in a project as a time limited pilot across named practices in Derby and Derbyshire.
The PHM approach requires health care organisations to work together with communities and partner agencies, for example, GP practices, community service providers, hospitals and other health and social care providers. These organisations will share and combine information with each other in order to get a view of health and services for the population in a particular area. This information sharing is subject to robust security arrangements.
As part of this programme, personal data about your health care will have all identifiers removed (like your name or NHS Number) and replaced with a code which will be linked to information about care received in different health care settings. If we see that an individual might benefit from some additional care or support, we will send the information back to your GP or hospital provider and they will use the code to identify you and offer you relevant services.
As part of this programme your GP and other care providers will send the information they hold on their systems to the North Of England Commissioning Support Unit (NECS). NECS are part of NHS England. More information can be found here https://www.necsu.nhs.uk
NECS will link all the information together. Your GP and other care providers will then review this information and make decisions about the whole population or particular patients that might need additional support. NECS work in partnership with a company called Optum to help them with this work. Both NECS and Optum are legally obliged to protect your information and maintain confidentiality in the same way that your GP or hospital provider is. More information about Optum can be found here www.optum.co.uk.
Health and Social Care Providers are permitted by data protection law to use personal information where it is ‘necessary for medical purposes’. This includes caring for you directly as well as management of health services more generally.
The PHM project is time-limited to 22 weeks. Once the project has completed all de-identified , information processed by NECS / Optum will be securely destroyed. This will not affect any personal information held by your GP or other health or social care providers.
Access to your personal information
Data Subject Access Requests (DSAR): You have a right under the Data Protection legislation to request access to view or to obtain copies of what information the surgery holds about you and to have it amended should it be inaccurate. To request this, you need to do the following:
- Your request should be made to the Practice. (For information from a hospital or other Trust/ NHS organisation you should write direct to them.
- There is no charge to have a copy of the information held about you
- We are required to provide you with information within one month
- You will need to give adequate information (for example full name, address, date of birth, NHS number and details of your request) so that your identity can be verified, and your records located information we hold about you at any time.
What should you do if your personal information changes?
You should tell us so that we can update our records please contact the Practice Manager as soon as any of your details change, this is especially important for changes of address or contact details (such as your mobile phone number), the practice will from time to time ask you to confirm that the information we currently hold is accurate and up-to-date.
You may ask us if you wish to have online access to your medical record. However, there will be certain protocols that we have to follow in order to give you online access, including written consent and production of documents that prove your identity.
Please note that when we give you online access, the responsibility is yours to make sure that you keep your information safe and secure if you do not wish any third party to gain access.
Third parties mentioned on your medical record
Sometimes we record information about third parties mentioned by you to us during any consultation, or contained in letters we receive from other organisations. We are under an obligation to make sure we also protect that third party’s rights as an individual and to ensure that references to them which may breach their rights to confidentiality, are removed before we send any information to any other party including yourself.
The only website this Privacy Notice applies to is the Surgery’s website. If you use a link to any other website from the Surgery’s website then you will need to read their respective Privacy Notice. We take no responsibility (legal or otherwise) for the content of other websites.
The Surgery’s website uses cookies. For more information on which cookies we use and how we use them, please see our Cookies Policy.
CCTV is installed on our practice premises covering both the external area of the building and the internal area excluding consulting rooms. Images are held to improve the personal security of patients and staff whilst on the premises, and for the prevention and detection of crime. The images are recorded onto an integral hard drive of the equipment and are overwritten on a rolling basis. Viewing of these digital images is password protected and controlled by the Practice Manager.
Our telephone system records all telephone calls. Recordings are retained for up to three years, and are used periodically for the purposes of seeking clarification where there is a dispute as to what was said and for staff training Access to these recordings is restricted to named senior staff.
Objections / Complaints
Should you have any concerns about how your information is managed at the GP, please contact the GP Practice Manager or the Data Protection Officer as above. If you are still unhappy following a review by the GP practice, you have a right to lodge a complaint with a supervisory authority: You have a right to complain to the UK supervisory Authority as below.
Information Commissioner:
Wycliffe house
Water Lane
Wilmslow
Cheshire
SK9 5AF
Tel: 01625 545745
If you are happy for your data to be used for the purposes described in this privacy notice, then you do not need to do anything. If you have any concerns about how your data is shared, then please contact the Practice Data Protection Officer.
If you would like to know more about your rights in respect of the personal data we hold about you, please contact the Data Protection Officer as below.
Data Protection Officer:
The Practice Data Protection Officer is Paul Couldrey of PCIG Consulting Limited. Any queries regarding Data Protection issues should be addressed to him at: –
Email: Couldrey@me.com
Postal: PCIG Consulting Limited
7 Westacre Drive
Quarry Bank
Dudley
West Midlands
DY5 2EE
Changes:
It is important to point out that we may amend this Privacy Notice from time to time. If you are dissatisfied with any aspect of our Privacy Notice, please contact the Practice Data Protection Officer.
Safeguarding our Vulnerable Patients
All staff at Hobs Moat Medical Centre are committed to protecting vulnerable patients no matter what their age. Safeguarding is sometimes thought to apply to children only, but older people also need protection at times. We hope you will find the information on this page helpful. The safeguarding lead for our Practice is Dr Alison Matthews. If you have any concerns, you can always speak to any member of our staff.
Hobs Moat Leaflet on Vulnerable patients can be picked up in the reception area or behind the reception desk please ask a member of staff to help you or click here for a copy.
Solihull Metropolitan Council is responsible for safeguarding services in Solihull
Protecting adults at risk
Ensuring physical, emotional and financial wellbeing
Everyone has the right to be treated with dignity and respect, whether they live on their own, with others, in a care/nursing care home, attend a day centre or are in hospital. Adults at risk are sometimes abused by people who should be looking after them.
Who is at risk?
We define an adult at risk as anyone aged 18 years or over who needs community care services, or who finds it difficult to take care of themselves or protect themselves against harm or exploitation. They might be elderly, physically or mentally ill, disabled, have learning difficulties or face other challenges.
What is abuse?
Abuse of an adult at risk is where someone in a position of trust hurts, harms or causes someone distress. It can include theft, bullying, verbal and racist abuse, threats, pressure about money or wills, unwanted sexual advances, physical abuse and neglect. Abuse can be stopped and even prevented, but this can only happen if someone knows about it.
How can we stop abuse?
Tell someone you trust, as soon as you can.
- Solhull MBC: 0121 704 8007 (outside office hours in an emergency: 0121 605 6060)
- Police: 101 (or 999 in an emergency)
- Elder Abuse Helpline: 0808 808 8141
- CQC: 0845 015 0120
You can print further information about what to do from here
Deprivation of Liberty Safeguards (DoLS)
Sometimes adults who are unable to make decisions about their care and treatment have to be cared for in a particularly restrictive way to keep them safe. The Mental Capacity Act 2005 has set out Deprivation of Liberty Safeguards (DoLS) to protect people in this situation.
Dols guidance leafet here
Domestic Abuse information here
South Solihull Primary care network
From 1st April all GP Practices are being asked to join with neighbouring practices to form clusters which are being called Primary Care Networks. These networks will be made up of GP practices that are close to one another in location to make a total network population of between 30,000 and 50,000 patients. This does not mean that these practices will be merging together, more that they will become the centres around which other NHS services will be wrapped, such as district nurses and social care.
So what does this mean for you as our patient and the practice you are registered with?
Four practices in our area, namely this one, St Margaret’s, Richmond Road and Grafton Road are coming together to form a Primary Care Network. We hope that by working more closely together with each other and the services that we all rely on to support our work, we will be able to jointly deliver an improved service to you, our patient.
As of 1st July, Primary Care Network has been approved by our local Clinical Commissioning Group and we have appointed a clinical director (Dr Vicky Matiopolou) to help our network focus on areas for improvement, and act as a link to the other Primary Care Networks in the area, the local hospitals, Health Watch, Solihull Council and the Clinical Commissioning Group. This will help us to influence how health and social care is delivered to our joint population.
One of the most important and hopefully noticeable improvement for you will be the creation of more extended hours appointments available outside of the usual Monday to Friday 8am to 6.30pm. This builds on the already very successful extended access hub which works out of Richmond Road surgery. In future, we hope to be able to offer a different range of appointments not just face to face but some telephone consultations as well as we know it can be difficult to have a discussion with your GP during the work day and possibly, on line.
Through another contract that we are all working to, all Practices in our network will gradually take on offering all their own appointments for patients who need to have blood tests. We hope to be able to offer some weekend and evening appointments through the hub for these tests to be taken.
We will also be employing a social prescriber who will support those isolated patients who need some support to integrate with the community and combat loneliness. The network will have a clinical pharmacist who will offer consultations to help patients understand their medication and resolve any problems they might be experiencing as well as help check patients’ medications when they are discharged from hospital
We are at the very beginning on an exciting journey that is part of the NHS long term plan for how care should be delivered to communities. Your Practice and its primary care network are committed to keeping you informed along every step of the way, so when we have more information or news, we will let you know.
In the meantime, if you would like to know more, you can always ask to speak to your practice manager
You might find this short video useful